CASES BY HENK
This page is aimed at general dentists and shows a broad range of very challenging cases that Henk has recently performed.
They demonstrate the complexity of root canal anatomy as well the potential for bony healing to occur, even with very large lesions. Henk embraced the need for using CBCT in endo long ago, and many cases demonstrate the use of 3D imaging.
This portfolio is an exhaustive demonstration of the challenges we face, and solve daily. For simplicity, it is seperated into surgical and non-surgical endodontics. In the unlikely event that non-surgical treatment or re-treatment is unsuccessful, the option for surgical treatment often exists. In tandem, these two treatment modalities lead to extreemly favourable outcomes.
NON-SURGICAL CASES
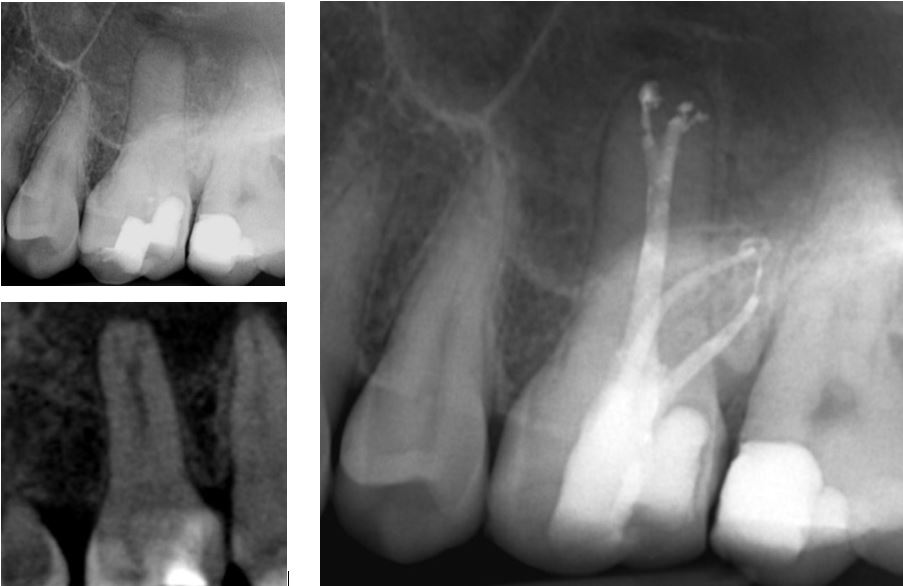
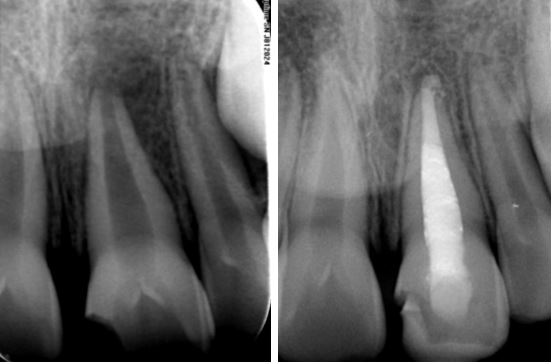
Severely Curved Roots
CASE 1
The challenges of treating this upper 6 with curved roots and calcified pulp and canals were identified by the referring dentist. Henk performed treatment and placed a core. The six month review radiograph with the tooth crowned, is shown.

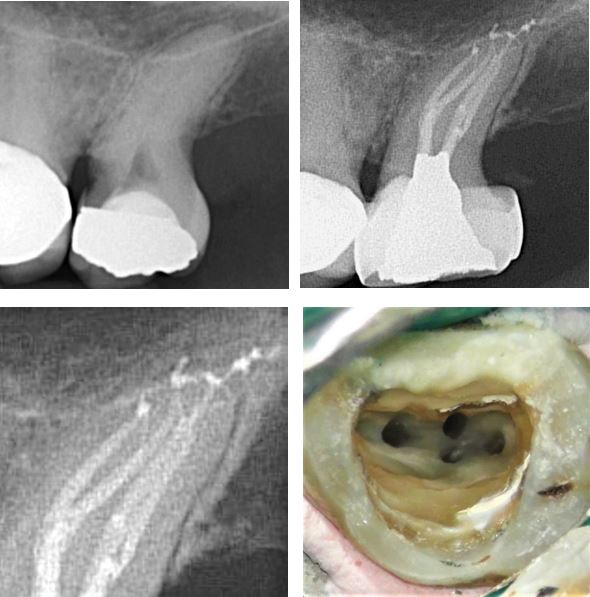
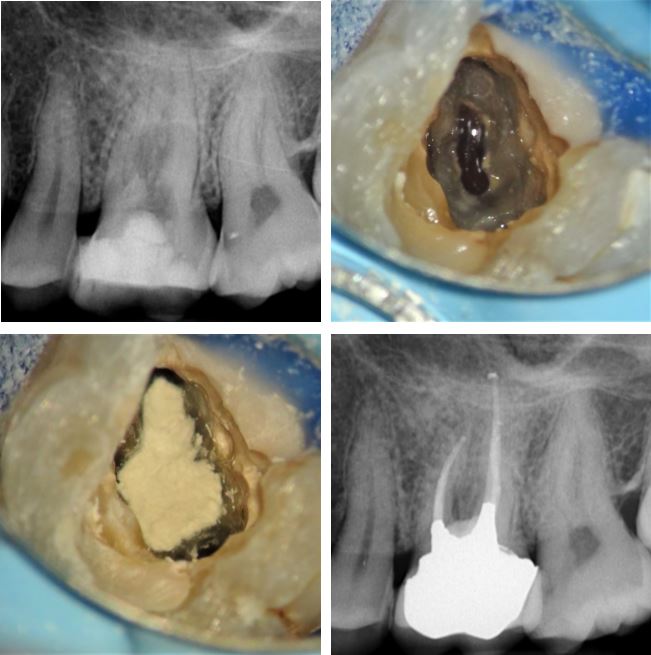
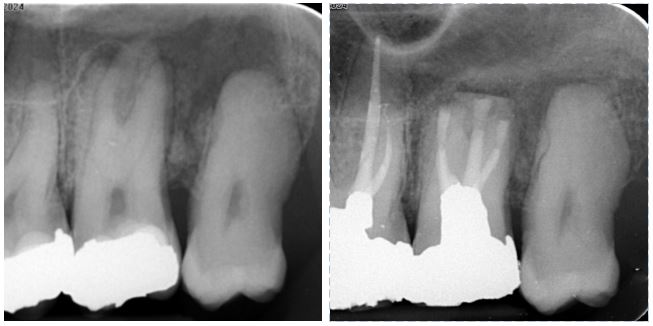
CASE 2
RCT was attempted on this upper 6. The extreme curvatures could not be negotiated and the patient was referred to Henk who performed treatment and restored the access cavity with a reinforced bonded resin. The patient was returned to the dentist for a definative cuspal protection restoration.
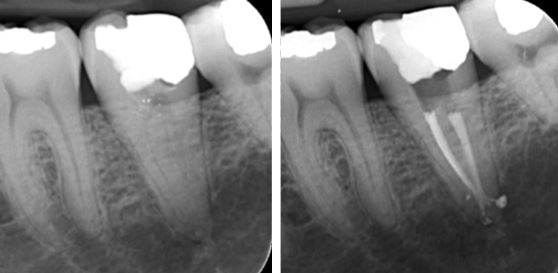
Deep Canal Divisions
CASE 1
This maxilliary first molar had a wide, blunt palatal root and this can hint at the presence of complex anatomy. A CBCT was taken and the sagittal slice clearly shows the anatomy that was duplicated on the final radiograph. The distal canal had restrictive access apically, only allowing for instrumentation with small hand files and hydraulic obturation with sealer (SystemB).
CASE 2
The lower premolars can be very challenging to treat as they comonly have deep canal divisions. This LR5 was referred as RCT had been attempted. Henk shaped, cleaned and obturated three canals in the apical third. A bonded resin core was placed for the referring dentist to prepare for a cuspal protection restoration
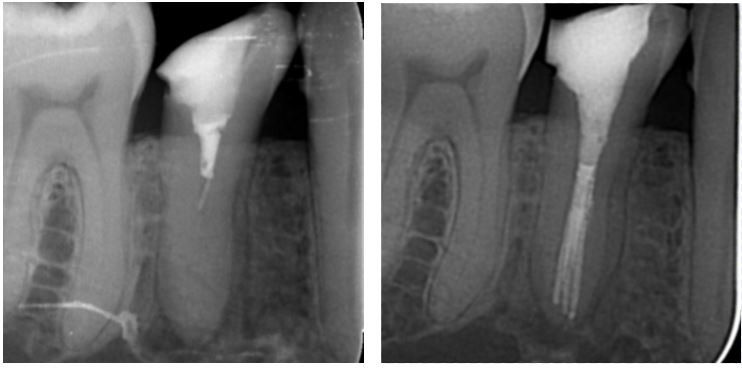
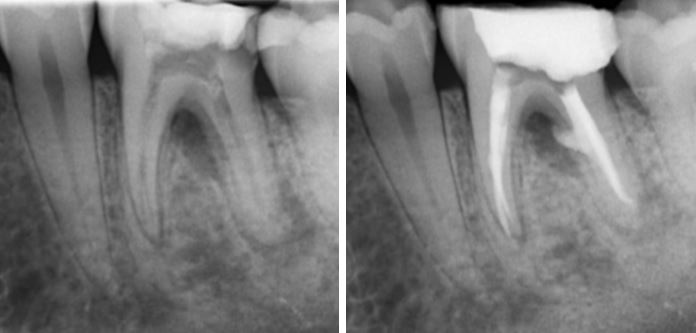
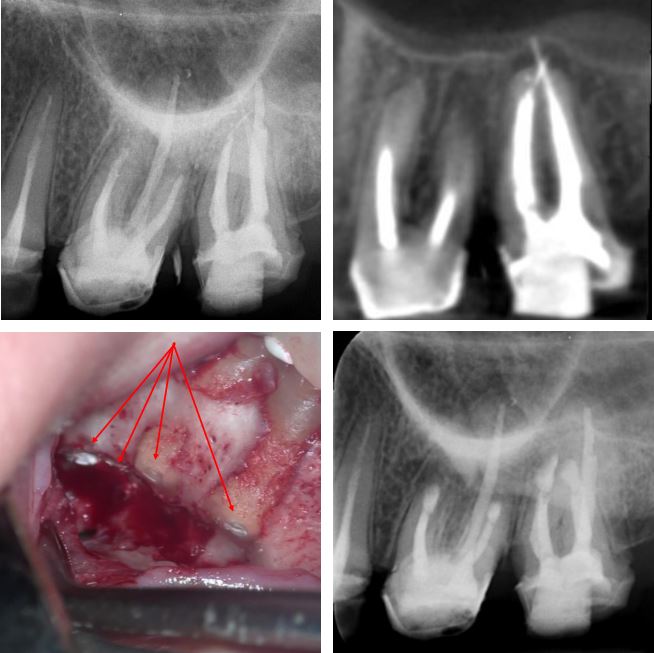
CASE 3
This UR6 developed symptomatic pulpitis secondary to a cracked cusp.The clinical picture was complex and a CBCT scan was used to confirm diagnosis. This showed deep bifurcation of the palatal canal. The axial slice section has arrows highting the mesial and distal branches of the root. Both branches were instrumented and bioceramics were used to obturate. A base of GIC was placed under a bonded resin core, ready for referring dentist to prepare for a definative restoration.
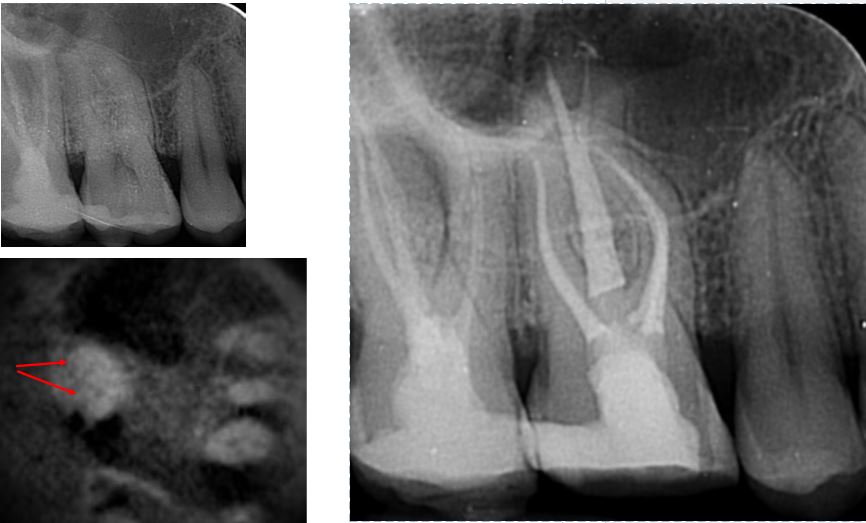
Unusual Root Canal Configurations
CASE 1
Lower premolars can have very challenging anatomy. This recently crowned LR5 developed an irriversable pulpitis and the pre-treatment radiograph hints at it having a mesial and distal root. A CBCT scan was taken and the sagittal slice (top right) confirms two seperate roots. The axial slice with yellow arrow at mesial root shows two canals in the distal root (red arrow). Following treatment through the crown, an amalgam access cavity restoration was placed to enhance shear resistance.
CASE 2
A heavily restored LL6 was referred as it required a crown and had a draining fistula associated with the periapical radiolucencies. Five canals (three mesial and two distal) were cleaned and dressed with calcium hydroxide for six weeks. On completion of the case the pulp chamber was cleaned with microabrasion and a bonded core was placed for the referring dentist to prepare. The final radiograph shows periapical healing underway. The filled canal orrifices are shown on the clinical photo.

CASE 3
An upper second, or possibly mesially drifted third molar with a single root and deep caries. The pre-treatment radiograph reveals nothing about the complex canal morphology in this tooth.This is fairly typical of single rooted molar teeth.
The clinical photo shows the shaped canal orrifices with very unusual and distinct mesial, distal, buccal and palatal canals. The completion radiograph shows apical delta and deep anastomoses between canals. The tooth was stabilized with a protective orthodontic band.
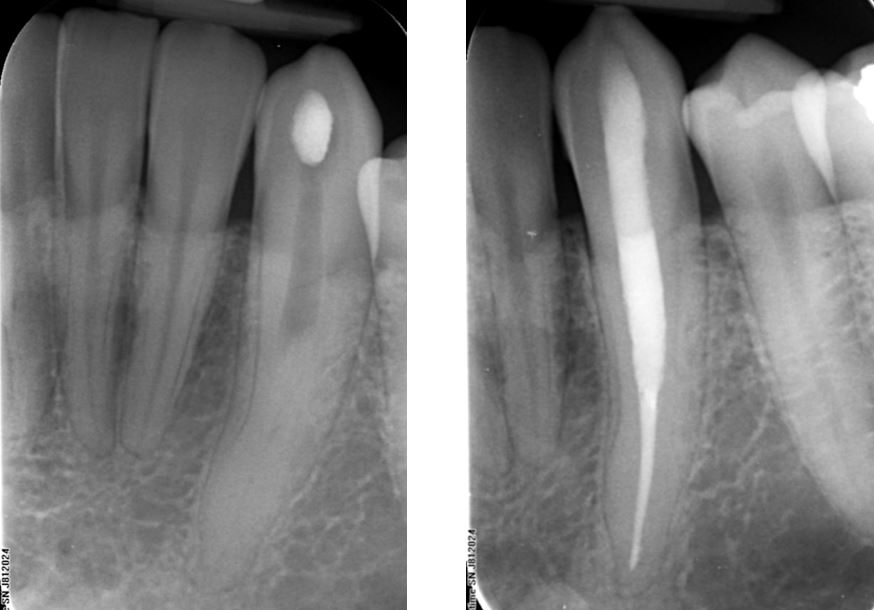
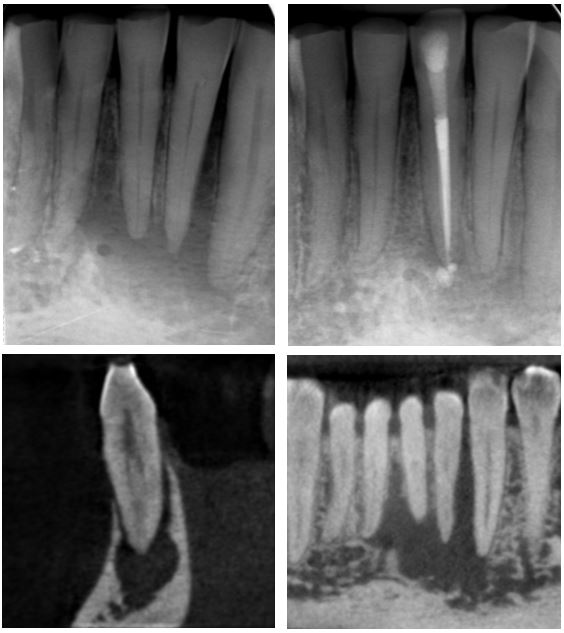
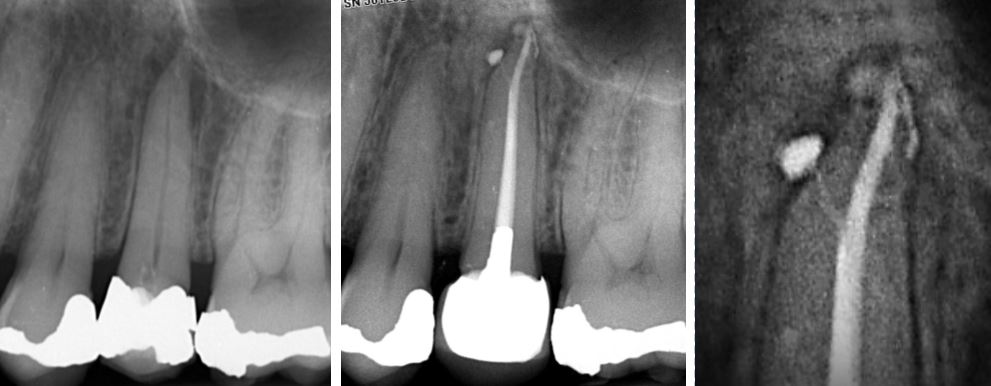
Teeth With Exceptionally Long Roots
CASE 1
Long roots are an endodontic challenge as they are difficult to instrument and irrigate to length, as well as obturate predictably.
This 32mm long lower canine shows unusual and sudden canal obliteration at mid-root level. Deep ultrasonic excavation to 20mm allowed for canal catheterization and completion of treatment.
The access cavity was restored with Fuji IX GIC.
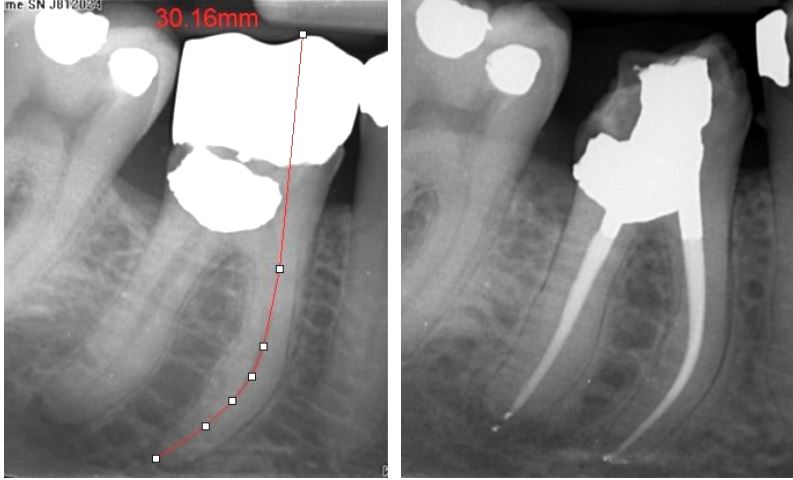
CASE 2
A crowned lower 6 with pre-treatment estimate length of 30mm. Secondary caries indicated crown removal and replacement following RCT. The large class V buccal amalgam had been placed in the buccal canal orrifices making this case more challenging. A temporary crown was placed and a six month review radiograph shows periapical healing so that a new crown could be placed.
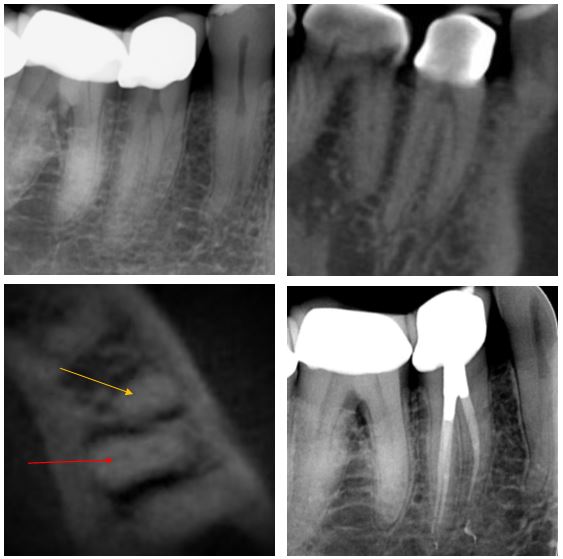
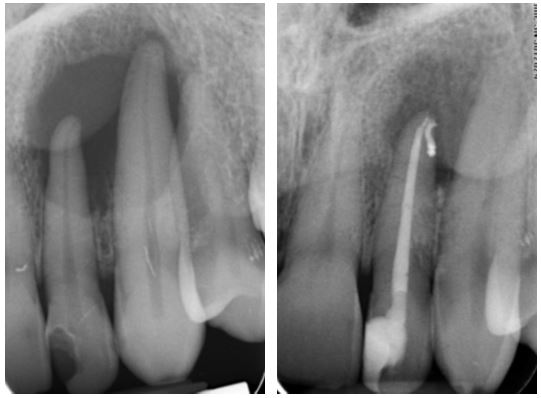
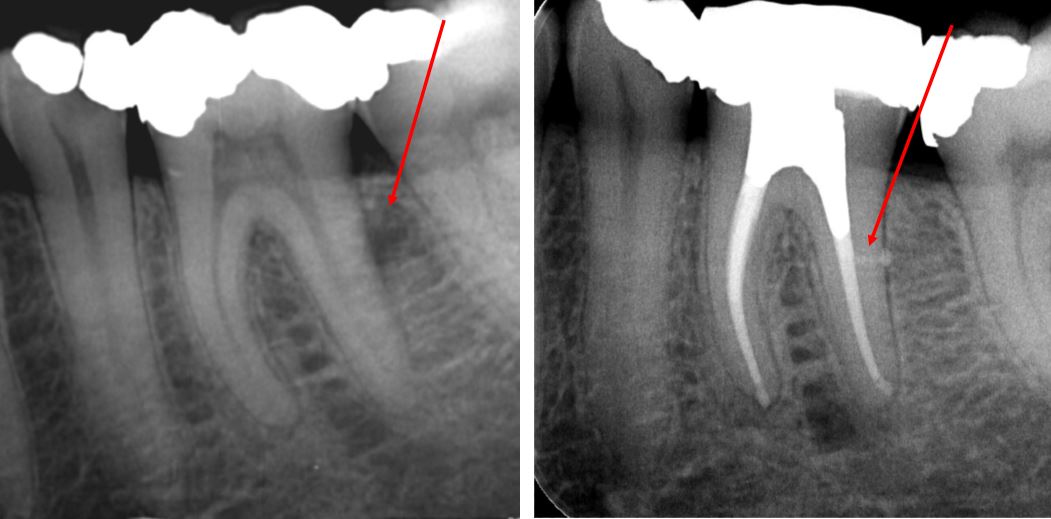
External Apical Resorption
CASE 1
This LR7 has a severely resorbed distal root, likely mediated by pressure from the impacted third molar (surface resorption) combined with inflamatory resorption typical of teeth with chronic periapical disease. An OPG was taken to rule out the presence of a dentigerous cyst and this showed the same clinical picture at LL7 (top right).
Definative treatment required RCT and removal of the impacted tooth. Bottom left shows post- treatment RCT and core placement. Bottom right shows six month follow-up radiograph once referring dentist had placed a crown, it shows good periapical healing preceding extraction of the LR8.

CASE 2
A more typical case of inflamatory external root resorption due to chronic periapical inflamation. As the periapical inflamation is an extension of pulpal disease, conventional endodontic management leads to good outcomes.
This crowned LR6 had secondary caries requiring caries removal and re-crowning. Following RCT, a core and tempory crown was placed. A three month review radiograph shows good healing underway so that the referring dentist could place a new crown.
Internal Resorption
CASE 1
This root treated upper 6 had an associated buccal draining fistula and large periapical radiolucency on the mesial root. The mesial root has a mid-root radiolucency that indicated a CBCT scan for resorption diagnosis. The sagittal and axial slice are shown. The axial slice with red arrow at the mesial root shows frank root perforation has not occured. A modified cleaning protocol with ultrasonic file activation in the mesial canal system was used, and the case was obturated with bioceramics prior to placing a GIC base and bonded composite core. The six month review radiograph shows excellent periapical healing underway.

CASE 2
A young patient with internal resorption of the palatal canal. Thermoplastic obturation allowed for a complete fill of the defect prior to restoring the access cavity with a deep base of GIC and a bonded restoration.

Calcified Pulp Canals
CASE 1
RCT was attempted by the referring dentist on the LL1 and LL2. As the pulp canals were obliterated, the canals were not located and the patient was referred.
Even with the use of a microscope and specialized ultrasonic instruments, such teeth are a challenge to treat. Henk located the canals and completed RCT by placing GIC plugs over the gutta percha and temporizing the access cavities.
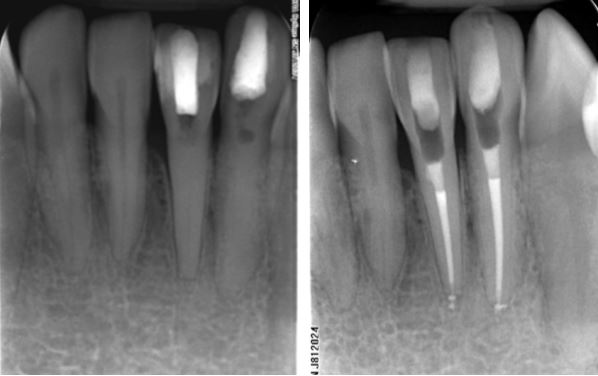
CASE 2
The challenges of performing endodontic treatment on this UL1 was recognised by the referring dentist who recommended that Henk perform the treatment. The post- treatment radiograph shows a conservative access cavity filled with GIC and minimal loss of tooth material.
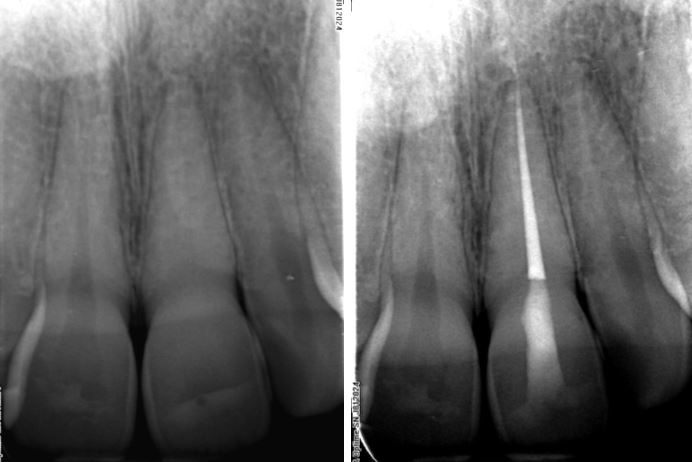
Healing of Large Periapical Lesions with Non-Surgical Treatment
CASE 1
Whilst large periapical radiolucencies are more likely to be radicular cysts than granulomas, they often respond well to non-surgical treatment.
This carious UL2 developed a draining fistula bucally and swellings both bucally and palatally, thus representing a “through and through” defect, i.e. loss of both the buccal and palatal cortices. Conventional RCT was performed and the 12 month review radiograph shows excellent osseous healing underway.
CASE 2
This case was referred due to buccal swelling associated with the lower incissors. The LL2 was suspected to be the the source of the problem as it had grade II mobility. The periapical radiograph shows a large radiolucency with significant loss of bone between LL2 and LL3. The coronal CBCT slice (bottom right) shows the lesion to extend from LR1 to LL3. Henk determined LL1 to be the endodontic source of the lesion. CBCT helped to exclude root fractures and the sagittal slice of LL1 (bottom left) shows this tooth to have buccal and lingual canals. RCT was performed and the six month review radiograph (top right) shows almost full resolution of the lesion
CASE 3
The root treated and crowned UR1 and UR2 were the source of a large radiolucency over their apices, with associated buccal and palatal swellings. A history of trauma indicated a CBCT scan to help exclude root fractures. This shows significant loss of the buccal cortex (reconstructed CBCT scan, bottom left), as well as cortical erosion palatally.
Inter-appointment calcium hydroxide dressings were placed for 12 weeks. The signs and symptoms resolved and the case was completed. The post-treatment radiograph (top right) shows early, but clear reduction in the size of the lesion and new osteoid bone deposits centrally after just 12 weeks.

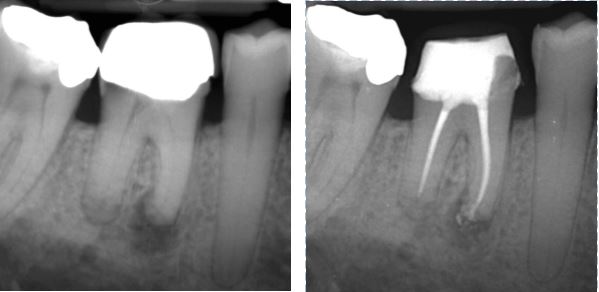
Perforation Repairs
CASE 1
Iatrogenic pulp floor perforations are not uncommon. Fortunatley, they generally respond very well to treatment. This upper 6 shows furcal bone loss due to a frank perforation a few months earlier. Henk performed RCT, perforation repair with MTA and an amalgam Nayyar core. The six month review radiograph shows furcal bone regeneration.
CASE 2
Root perforations are quite uncommon but can occur with endodontic instrumentation or post-space preparation. This lower 6 has significant furcal bone loss due to perforation of the distal root. The canals were obturated with bioceramic materials, and the perforation was repaired with bioceramic putty before temporizing.
Lateral Canals
CASE 1
The lateral radicular radiolucency on the distal root of this lower 6 was the cause of of a periradicular abscess. The three month review radiograph shows complete healing of the lesion with the associated lateral canal filled. Bioceramics were used in this case. While bioceramic sealers are superb in many ways, they are not yet very radiopaque.
CASE 2
This upper 5 shows good periapical healing at six month review. The magnified periapical view shows lateral canals filled with bioceramic sealer.
Open Apices
CASE 1
Immature teeth with endodontic infections are, generally, treated using an “apexification” procedure to provide an apical barrier. For this upper central in an 8 year old, an MTA apical plug was placed and the rest of the canal backfilled with thermoplastic g.p. and the access restored with GIC. The 6 month review radiograph shows periapical healing underway.
Case 2
Preventing extrusion of apical plug matrial in cases with a very open apex, such as in this nine year-old, is challenging. In this case bioceramics were used for the apical plug and the canal was then backfilled with thermoplastic g.p. and AH Plus sealer. A shallow GIC orrifice plug was placed to enhance the seal before temporizing.

CASE 3
This upper central incissor has a fairly mature root, however the apex was gauged to a size too large for predictable sealing with g.p. and sealer. Bioceramic putty was used for an apical plug and the remaining canal filled with bioceramic g.p.and sealer. A base of GIC was placed at the ECJ level in preparation for future internal whitening and the access temporized with IRM, as seen on the 6 month review radiograph.

Merging and “C” Shaped Roots
CASE 1
“C” shaped canals are mostly found in lower second molars, however, they are also found in upper molars and rarely in lower premolars. There is one root with a “C” shaped axial cross-section and merging canals, making them difficult to shape, clean and fill well. This lower 7 was completed with a base of GIC over the g.p. prior to placing a core and crown.

CASE 2
Similar to case 1 above, except after the canals merge, they seperate and have multiple portals of exit.
SURGICAL CASES
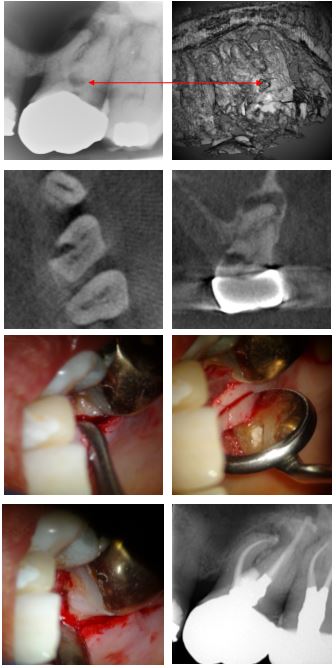
Cervical Root Resorption Treated With Aid Of CBCT
Case 1 – Molar Tooth
This gentleman presented with discomfort from the left hand side posterior teeth. A periapical radiograph showed periapical radiolucencies associated with UL6 and UL7. A cervical radiolucency, typical of cervical root resorption was also obvious. This indicated CBCT investigation and the associated 3D rendered image and corresponding lesion indicated by the red arrows, is shown. The next two CBCT slices are the axial and coronal views of the lesion.
The RCT was performed and the canal orrifices and access cavity filled with a temporary material. The clinical photos show the surgically exposed lesion prior to, and following curretage. The defect was restored with Geristore®, a resin-ionomer. On a second visit the access cavity was restored with amalgam for shear resistance.
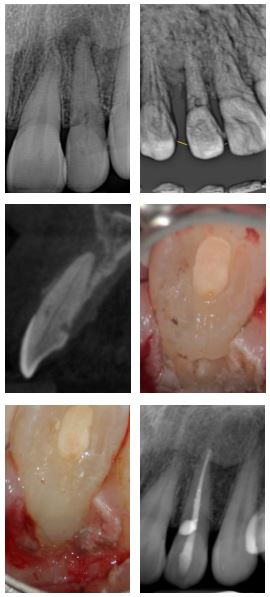
CASE 2
This unrestored UL2 developed a periapical abscess. The referring dentist noticed a small cervical radiolucency and referred the patient to Henk for management. Cervical root resorption was suspected and confirmed with CBCT. Following RCT, a palatal flap was raised and the defect cleaned and restored with Geristore®. A six month review radiograph confirms periapical healing (bottom right).
It can be challenging to diagnose external root resorption on a periapical radiograph. However, by comparison, internal root resorption has a significantly lower prevalence than external root resorption.
Intentional Replantations
CASE 1
The outcomes for intentional replantations is generally very good indeed. This treatment modality is used where conventional apical surgery is contraindicated or high risk. This UL7 was the source of a palatal draining fistula and large radiolucency over the UL7 and UL8. Signs and symptoms did not resolve after shaping, cleaning and calcium hydroxide dressing. The decision was taken to remove the tooth, perform apical resection with retrograde MTA plugs, and the tooth replanted. Signs and symptoms resolved shortly therafter and the 4 month review radiograph shows excellent periapical resolution underway.
CASE 2
This root treated and post -crowned LR5 developed symptomatic apical periodontitis. The patient was an elderly lady who couldn’t lolerate a lengthy re-RCT appointment. The decision to perform a 15 minute replantation procedure, as in case 1 above, was taken. The 12 month review radiograph shown a new PDL becoming established apically.

Apical Micro-Surgery
CASE 1
In this case, the temporized UL6 and UL7 had already been re-treated before the patient was referred to Henk for management as the teeth had remained symptomatic. CBCT scan revealed normal palatal root PDL’s, but apical lesions on the buccal roots of both teeth with over-extension of the g.p. on the UL7. The challenge of accessing the UL7 roots was reduced by resection of the UL6 apices. Ultrasonic retro-preparation preceded placement of bioceramic apical plugs (red arrows).
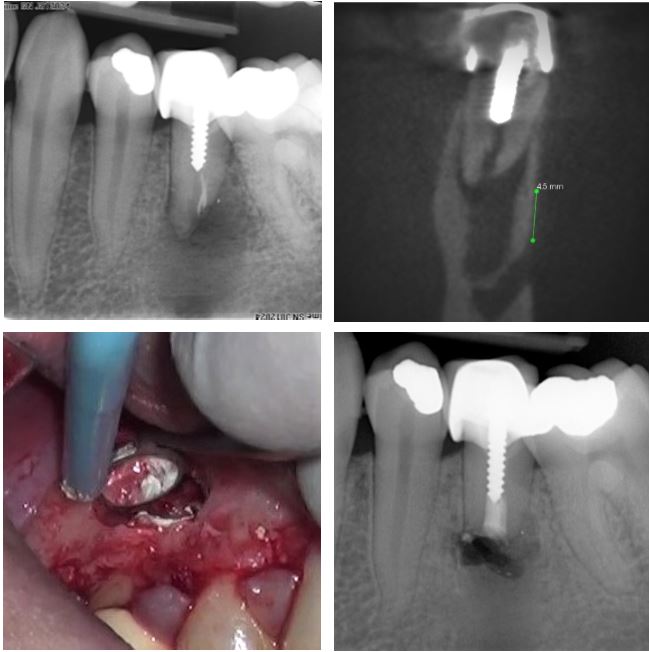
CASE 2
This recently post-crowned UR3 developed a periapical abscess and the patient opted for surgery, rather than re-treatment. The sagittal CBCT slice shows that the lesion has eroded both the buccal and palatal cortices. This indicates the need for grafting the bone cavity to limit the risk of healing by scar, rather than bone. Bottom left shows the radiograph taken post-treatment with bioceramic apical plug placed up to the apical extent of the post as well as the grafted defect. Bottom right is the six month review radiograph showing excellent osseous repair.
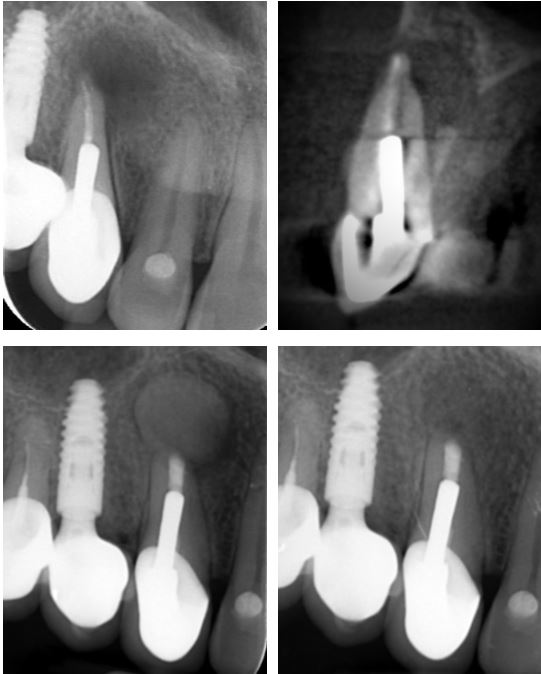
CASE 3
This post-crowned LL5 has a wide, obliquely resorbed “apex.” Apical micro-surgery produces more predictable results in such cases than re-RCT. The coronal CBCT slice with measurement, shows about 5mm leeway to the mental neurovascular bundle, allowing for surgical access. Bottom left shows the site and retroprep following placement of a bioceramic apical plug. Bottom right post-treatment shows a very satisfactory outcome with a good prognosis.
Call Us for an Appointment
Make An Online Enquiry





